
Heart disease poses a significant health challenge in Australia, encompassing conditions like coronary heart disease, stroke, and various cardiovascular ailments. Understanding the prevalence and impact of heart disease is crucial to addressing its far-reaching implications on individuals and the healthcare system. By delving into the statistics surrounding heart disease, we gain valuable insights into the scope of the problem and are empowered to take informed action through preventive measures and interventions. The main objective of this overview is to explore the prevalence, risk factors, and consequences of heart disease, enabling us to develop effective strategies to combat this health threat and improve the cardiovascular well-being of the Australian population. By confronting heart disease head-on, we can pave the way for a healthier future for all Australians, easing the burden on healthcare resources and fostering a society where heart health prevails.
Types of heart disease
Cardiovascular disease (CVD) encompasses various heart and blood vessel-related conditions, affecting individuals in many ways. Common types of CVD in Australia include coronary heart disease, stroke, and heart failure, with each state posing unique challenges. Atherosclerosis, characterised by the buildup of fatty deposits in arteries, is a crucial factor contributing to many forms of CVD, ultimately restricting blood flow to the heart or brain.
Coronary heart disease, or ischaemic heart disease, is the most prevalent form of CVD, presenting in two primary clinical forms: heart attack and angina. Heart attacks, or acute myocardial infarctions, are life-threatening events caused by sudden blockages in blood vessels supplying the heart. Angina, on the other hand, is characterised by chest pain resulting from reduced blood flow to the heart.
In addition to coronary heart disease and stroke, other noteworthy forms of CVD impact individuals differently. Heart failure occurs when the heart weakens, leading to reduced blood circulation. Cardiomyopathy, associated with straining the entire heart muscle or a significant part of it, can occur alongside heart failure due to various factors like coronary heart disease, hypertension, viral infections, and excessive alcohol consumption. Atrial fibrillation, a disturbance in the heart's electrical system, causes an irregular heartbeat and reduces the heart's efficiency in pumping blood. Peripheral arterial disease primarily affects the arteries leading to the legs and feet, resulting in reduced blood flow to these areas. Hypertensive disease, caused by severe or prolonged high blood pressure, can lead to various heart and organ-related complications. Furthermore, acute rheumatic fever, an autoimmune response to a streptococcus bacterial infection, can cause inflammation throughout the body, including the heart, brain, skin, and joints, potentially resulting in rheumatic heart disease with permanent damage to the heart muscle or valves. Lastly, congenital heart disease refers to various heart defects present at birth, such as malformation of heart valves or blood vessels.
Addressing the diverse spectrum of CVD requires targeted prevention, early detection, and effective management strategies. Fostering heart-healthy lifestyles, raising awareness about risk factors, and providing timely medical interventions are essential in combating the impact of CVD on public health and improving the well-being of individuals affected by these conditions.
How many Australians have heart, stroke and vascular disease?
Heart disease encompasses a range of cardiovascular conditions, including coronary artery disease, heart failure, arrhythmias, and valvular disorders. The risk of developing heart disease increases with age, affecting both men and women, although certain risk factors may vary between genders.
The prevalence of heart, stroke, or vascular disease-related conditions in Australia is a cause for great concern, with an astounding 1.2 million individuals aged 18 and over (equivalent to 6.2% of the adult population) reported to be affected in 2017–18 (Australian Institute of Health and Welfare, n.d.). These numbers highlight the significant impact of cardiovascular health issues on the nation's adult population and emphasise the urgent need for preventive measures and improved healthcare strategies. Addressing this widespread health challenge is crucial to enhance the well-being of Australians and reduce the burden of heart, stroke, and vascular diseases on individuals, families, and the healthcare system as a whole.
Hospitalisation
In 2020–21, the burden of cardiovascular disease (CVD) on Australia's healthcare system was substantial, with 600,000 hospitalisations recorded, where CVD was the principal diagnosis. This figure translates to 2,300 hospitalisations per 100,000 population, significantly impacting the nation's health. (Australian Institute of Health and Welfare, n.d.)
The 600,000 CVD-related hospitalisations accounted for 5.1% of all hospitalisations in Australia during the same period. Among these cases, 90% (542,000 hospitalisations) were classified under acute care, focusing on surgical, diagnostic, or therapeutic procedures to treat illnesses or injuries.
The data revealed a distribution of CVD-related hospitalisations with varying principal diagnoses. Coronary heart disease topped the list at 27%, followed by atrial fibrillation at 13%, heart failure and cardiomyopathy at 12%, and stroke at 11%. Additionally, peripheral arterial disease accounted for 5.5% of hospitalisations, hypertensive disease for 2.7%, and rheumatic heart disease for 0.8%.
These statistics shed light on the gravity of CVD's impact on Australia's healthcare resources, patients, and families. As we face the challenges posed by this significant health concern, it becomes paramount to prioritise preventive measures, early detection, and effective management strategies to alleviate the burden of CVD and improve the population's overall well-being.
Age and Gender
In the fiscal year 2020–21, hospitalisation rates with cardiovascular disease (CVD) as the principal diagnosis revealed significant gender and age disparities. After accounting for differences in age structure, rates were 1.6 times higher for males compared to females, with higher rates among males across all age groups. Most CVD hospitalisations (84%) occurred in individuals aged 55 and over, with the highest rates in the 85 and over age group, reaching 20,200 per 100,000 population for males and 15,700 per 100,000 for females. Over the period from 2000–01 to 2020–21, the number of acute care hospitalisations with CVD as the principal diagnosis increased by 38%, from 393,000 to 542,000. However, the age-standardised rate declined by 16% from 2,070 to 1,740 per 100,000 population. Throughout this period, CVD hospitalisation rates were consistently higher for males than females, with both genders experiencing similar declines.
Mortality
In 2021, the alarming impact of cardiovascular disease (CVD) on mortality was evident, with 42,700 deaths attributed to it, accounting for 25% of all recorded deaths. The rate of CVD-related deaths stood at 166 per 100,000 population, underscoring the severity of the issue. Although CVD ranked as the second leading cause of death, following cancers (30% of all deaths), it surpassed other primary causes, including diseases of the respiratory system, external causes, mental and behavioural disorders, and nervous system conditions.
When examining cases where CVD was listed as the underlying cause of death in 2021, coronary heart disease was the most prevalent, contributing to 41% of deaths. Stroke followed closely at 20%, while heart failure and cardiomyopathy accounted for 11% of deaths. Additionally, hypertensive disease and atrial fibrillation represented 5.7% of CVD-related deaths. Peripheral arterial disease and rheumatic heart disease accounted for 4.5% and 0.8% of deaths, respectively.
The burden of disease
In 2022, Coronary Heart Disease (CHD) emerged as the leading specific cause of duty in Australia, resulting in 306,000 years of healthy life lost, equivalent to 9.0 daily per 1,000 population. The load was higher in males, accounting for 205,000 disability-adjusted life years, compared to 100,000 disability-adjusted life years in females. The impact of CHD increased significantly from age 45 onwards, surging from 6.6 per 1,000 among people aged 45–49 to 191 per 1,000 among those aged 95–99 (AIHW 2022a).
CHD constituted 5.5% of Australia's total disease burden, comprising 8.9% of the fatal and 2.4% of the non-fatal burdens.
Over the period between 2003 and 2022, CHD experienced a substantial decline in burden, reducing by 28% (118,000 disability-adjusted life years ). The CHD rate also saw a remarkable reduction of 57%, dropping from 21 to 9 disability-adjusted life years per 100,000 population. CHD's fatal and non-fatal burdens decreased by 59% and 48%, respectively. This positive trend has been attributed to various factors, including population growth, ageing, and improvements in disease management (AIHW 2022a).
Expenditure on Cardiovascular Disease
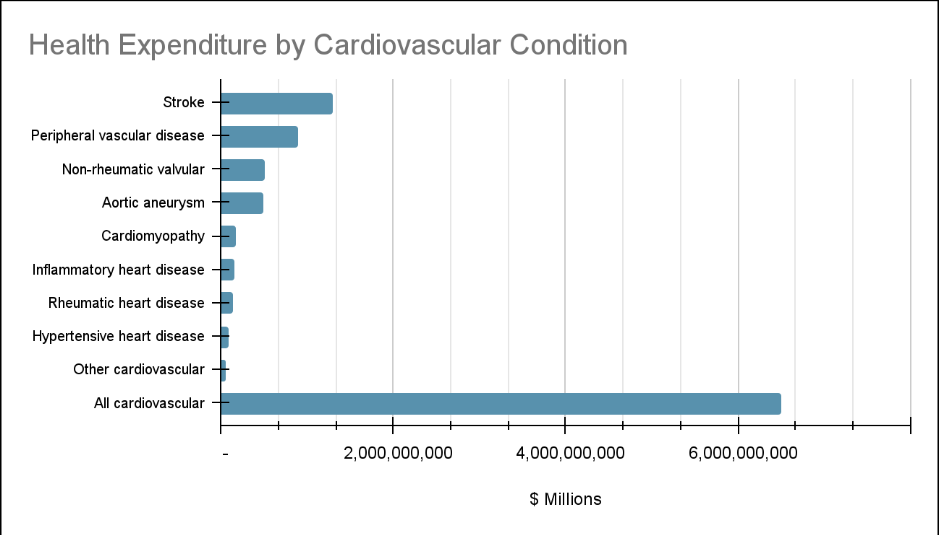
In 2019–20, cardiovascular disease (CVD) accounted for approximately 9.1% of the total allocated spending in the Australian health system, amounting to a substantial $12.7 billion.
Most of the allocated funds for CVD, around 69% or $8.8 billion, were directed towards hospital services, reflecting the significant burden of CVD on the healthcare system.
Regarding the demographic distribution, the highest expenditure on CVD in 2019–20 was observed among males aged 65–74 and females aged 75–84, indicating that these age groups bear a considerable share of the financial burden related to cardiovascular disease.
This significant investment in CVD management underscores the importance of addressing this health issue. It highlights the need for effective preventive strategies and healthcare interventions to mitigate cardiovascular disease's impact on individuals and the healthcare system.
In 2019–20, cardiovascular disease (CVD) accounted for approximately 9.1% of the total allocated expenditure in the Australian health system, amounting to a substantial $12.7 billion. This made CVD the disease group with the second highest expenditure, following musculoskeletal disorders ($14.6 billion). The significant investment in CVD reflects its status as a leading cause of death and a major contributor to Australia's overall disease burden.
Among the various cardiovascular conditions, coronary heart disease (CHD) emerged as the most expensive, with approximately 18.8% of the CVD expenditure totalling $2.4 billion. Atrial fibrillation (AF) and stroke followed as the subsequent costly conditions, accounting for 10.3% ($1.3 billion) and 7.0% ($894 million) of the CVD expenditure, respectively. (AIHW 2022a).
These figures highlight the substantial financial resources dedicated to managing cardiovascular disease in Australia. As CVD continues to impose a significant health and economic burden, effective prevention strategies and targeted healthcare interventions are paramount in reducing its impact and improving the overall cardiovascular health of the population.
These statistics highlight the urgent need for effective preventive measures, early detection, and improved management strategies to combat CVD’s devastating impact on mortality. Raising awareness about risk factors, promoting heart-healthy lifestyles, and ensuring access to quality healthcare are crucial steps towards reducing the burden of cardiovascular disease and safeguarding the population’s well-being.
Reducing the burden of cardiovascular diseases (CVDs) necessitates incorporating effective management interventions into universal health coverage packages. Many health systems worldwide require significant investment and reorientation to tackle CVDs efficiently.
Evidence from 18 countries indicates that hypertension programs can be successfully and cost-effectively implemented at the primary care level, reducing coronary heart disease and stroke cases. (Cardiovascular Diseases (CVDs), 2021) Ensuring patients with CVDs have access to appropriate technology and medication is crucial. Essential medicines like aspirin, beta-blockers, angiotensin-converting enzyme inhibitors, and statins should be readily available.
Prompt management of acute CVD events, such as heart attacks or strokes, is imperative. In some cases, surgical operations become necessary to treat CVDs, including coronary artery bypass, balloon angioplasty (opening blockages with a small balloon-like device threaded through an artery), valve repair and replacement, heart transplantation, and artificial heart operations.
Furthermore, medical devices play a vital role in treating certain CVDs. These devices include pacemakers, prosthetic valves, and patches for closing holes in the heart. By ensuring access to these interventions, promoting preventive measures, and raising awareness about heart-healthy lifestyles, we can significantly reduce the burden of cardiovascular diseases and improve overall public health.
To reduce the burden of cardiovascular diseases (CVD), several lifestyle and behaviour modifications are essential. Globalisation, socio-economic changes, and unemployment have influenced the CVD epidemic, increasing health inequalities. Key components of human behaviour, such as diet, exercise, smoking, and job-related features, play a significant role in these disparities. Addressing these factors through lifestyle interventions can substantially improve CVD prevention and management.
Protecting Yourself Financially From Cardiovascular Disease
Undoubtedly, medical expenses are escalating rapidly, driven by time and inflation. Dealing with a heart ailment is not a financial burden everyone can easily bear, especially in critical emergencies. Beyond the fundamental hospitalisation and medical costs, there are numerous other expenses, such as doctor's consultation fees, room charges, and additional medical costs. In some cases, even surgery may be necessary.
A heart care policy or heart attack insurance is essential to protect yourself from the potential financial strain caused by heart-related issues. In emergencies, these insurance policies offer coverage and aid in paying for medical bills related to sudden cardiovascular problems. They serve as a safety net, preventing you from facing significant financial burdens during medical crises. With the right insurance coverage, you can have peace of mind, enabling you to concentrate on your health and recovery without worrying about financial implications.
The costs related to cardiovascular treatments are substantial, and they constitute one of the most significant expenses at the national level. Managing cardiovascular disease, including heart attacks, strokes, and other related conditions, involves a range of medical interventions, hospitalisations, medications, and follow-up care. These expenses can quickly add up and place a considerable financial burden on individuals and families.
In the face of such potential medical emergencies, you must protect yourself financially. A heart attack can strike suddenly, leaving little time for financial preparation. Therefore, having a robust financial plan can offer peace of mind and help you cope with the financial repercussions of a cardiovascular event.
Here are some steps individuals can take to strengthen their financial security in a cardiovascular emergency:
Health Insurance: Investing in a comprehensive health insurance plan that covers cardiovascular treatments is essential. Health insurance can help offset the costs of hospitalisations, surgeries, medications, and follow-up visits, significantly reducing out-of-pocket expenses.
Being well-informed about the best health insurance policy is crucial to avoid pitfalls. Many individuals make the mistake of choosing a plan without thoroughly reading the fine print, only to discover later that certain ailments are not covered or they face significant out-of-pocket expenses. To prevent such situations, comparing your insurance plan with Health Deal is essential. Taking advantage of Health Deal's expertise can ensure that you make an informed decision and have the appropriate coverage for any potential health issues that may arise. Compare now to ensure you’ve got the exact coverage you need.
Emergency Fund: Building and maintaining an emergency fund is vital. This fund should ideally cover several months' worth of living expenses, including potential medical costs. Having a financial cushion can provide relief during times of crisis and prevent the need to take on high-interest debts.
Budgeting and Financial Planning: Individuals should take proactive financial measures to safeguard against potential financial strain caused by cardiovascular issues. A well-structured budget enables close monitoring of income and expenses, identifying areas for cost reduction and freeing up funds for savings and emergency preparedness. Adopting a healthy lifestyle, including regular exercise, a balanced diet, and avoiding tobacco and excessive alcohol consumption, significantly lowers the risk of cardiovascular diseases, potentially reducing long-term medical expenses. Long-term financial planning, such as contributing to retirement accounts and investment vehicles, ensures financial stability during increased health-related expenses. Seeking advice from a financial advisor can provide personalised guidance to address the specific financial challenges posed by cardiovascular treatments. By implementing these strategies, individuals can enhance their financial security, allowing them to focus on their health and recovery during potential cardiovascular emergencies.
Individuals can better prepare for unforeseen medical emergencies, including cardiovascular events, by enhancing financial security. Being proactive about financial planning helps alleviate the stress of potential financial burdens and enables individuals to focus on their recovery and overall well-being.
The statistics surrounding heart disease in Australia paint a clear and urgent picture of the formidable health challenge it poses. Heart disease remains the leading cause of death in the country, impacting a significant portion of the adult population. It burdens the healthcare system with a substantial number of hospitalisations, and its impact on mortality underscores the severity of the issue. Addressing heart disease head-on requires a multi-faceted approach, including preventive measures, early detection, and effective management strategies.
The prevalence of various types of cardiovascular disease, such as coronary heart disease, stroke, and heart failure, demands comprehensive understanding and targeted interventions. Atherosclerosis, characterised by fatty deposits in arteries, is crucial in restricting blood flow and causing many forms of heart disease.
The burden of heart disease falls disproportionately on certain age groups, with individuals aged 55 and over experiencing the highest hospitalisation rates. Furthermore, there are significant gender disparities, with males consistently experiencing higher hospitalisation rates than females.
The financial burden of managing cardiovascular disease is substantial, with billions of dollars allocated to address the healthcare needs associated with heart-related conditions. Coronary heart disease is the most expensive cardiovascular condition, followed by atrial fibrillation and stroke. Comparing health insurance plans is essential for achieving financial awareness and making informed decisions about one’s healthcare coverage. Without proper comparison, individuals may end up with plans that do not adequately meet their specific needs, leading to unexpected financial burdens during medical emergencies or when seeking treatment. Understanding the extent of coverage, co-payments, deductibles, and other out-of-pocket expenses is crucial to avoid unpleasant surprises and effectively plan for healthcare costs. By comparing different health insurance options, individuals can identify the most suitable plan that aligns with their healthcare requirements and financial capabilities, ensuring they are well-prepared to manage medical expenses.
Moreover, financial awareness in health insurance includes recognising the long-term implications of policy choices. A well-chosen insurance plan addresses immediate healthcare needs and contributes to proactive financial planning for future medical expenses, such as chronic conditions or preventive care. It allows individuals to explore additional benefits and value-added services offered by various insurers, enabling them to make comprehensive decisions about their health coverage. With the help of online insurance comparators like Health Deal and guidance from trained health insurance agents, comparing and changing plans is fast and straightforward. Overall, being financially aware of health insurance options empowers individuals to take control of their healthcare costs, secure their financial well-being, and achieve peace of mind for themselves and their families.
Investing in preventive strategies, early detection programs, and improved management interventions to combat heart disease effectively is crucial. Implementing hypertension programs at the primary care level has reduced coronary heart disease and stroke cases. Ensuring access to essential medications and medical interventions and promoting heart-healthy lifestyles can significantly reduce the burden of heart disease.
Understanding heart disease statistics is crucial for formulating effective public health policies and interventions to combat this major health threat. By raising awareness, implementing preventive measures, and improving healthcare access, we can create a healthier future for all Australians, reducing the burden of heart disease on individuals, families, and the healthcare system. We can improve cardiovascular well-being through collective efforts and informed action and promote a society where heart health prevails.

 Single
Single Couple
Couple Family
Family Single Parent
Single Parent